What is the cornea?
You can think of the cornea as the front of a camera’s lens. The cornea is a clear, dome-shaped surface that covers the front of the eye and acts as the eye’s 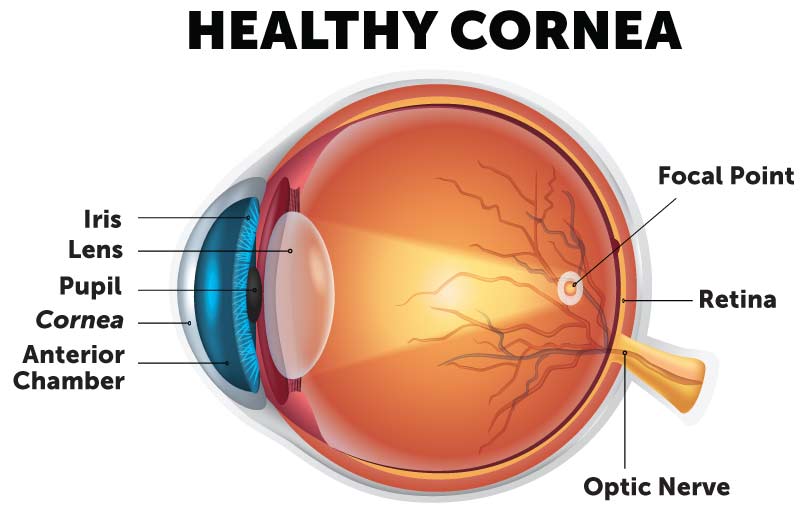 outermost layer. Like a camera lens, your eye’s cornea is responsible for controlling how light is focused. A healthy, clear and regularly shaped cornea works with your eye’s lens to refract light onto your retina in the back of the eye. The retina then acts as a processing center, helping your brain to make sense of what you see. Together, these vital functions help you see clearly and focus on objects. The cornea is responsible for up to seventy-five percent of the eye’s total focusing power, and cornea eye disease can interrupt its function and disrupt your eyesight. Because the cornea is so crucial to clear vision, any abnormality to the shape or composition of the cornea can affect your ability to see clearly and can interfere with performing daily activities.
outermost layer. Like a camera lens, your eye’s cornea is responsible for controlling how light is focused. A healthy, clear and regularly shaped cornea works with your eye’s lens to refract light onto your retina in the back of the eye. The retina then acts as a processing center, helping your brain to make sense of what you see. Together, these vital functions help you see clearly and focus on objects. The cornea is responsible for up to seventy-five percent of the eye’s total focusing power, and cornea eye disease can interrupt its function and disrupt your eyesight. Because the cornea is so crucial to clear vision, any abnormality to the shape or composition of the cornea can affect your ability to see clearly and can interfere with performing daily activities.
The cornea also acts as a barrier. As one of your eye’s first lines of defense, the cornea helps shield the rest of the eye from germs, dust and other hurtful matter that can cause cornea eye disease, an inflamed cornea, corneal abrasions or other corneal injuries. Although the cornea is clear and seems to lack substance, it is a strong and durable highly organized group of cells and proteins. However, the cornea is very sensitive and unlike most tissues in the body, the cornea contains no blood vessels to nourish or protect it against infection. Rather, the cornea receives its nourishment from the tears and clear fluid (aqueous humor) that fills the front of the eye. For this reason, it is important that the tears you produce are healthy and do not evaporate quicker than necessary, otherwise you may experience dry eye symptoms and increase the risk of corneal injury.
What is cornea eye disease?
There are a wide variety of conditions and diseases that can affect the cornea, ranging from temporary and minor to serious and permanent. No matter the severity, all corneal diseases may negatively impact your vision, comfort and daily life. The most common types of corneal diseases include:
-
Infections
-
Trauma
-
Allergies
-
Dryness
Hereditary corneal disease can include conditions such as Fuchs dystrophy, keratoconus and other corneal dystrophies. Depending on the condition, symptoms may develop slowly or come on suddenly and cause immediate pain and vision issues. Since causes and conditions vary, treatment for corneal eye disease also depends on the cornea condition or disease diagnosis. In some minor cases, your cornea can repair itself; other conditions may require medical treatment such as antibiotics or surgery such as cross-linking or corneal transplantation.
Cornea Eye Diseases Affecting the Corneal Surface
The superficial layers of the cornea surface are very important. In addition to the tear layers, the epithelium and anterior stromal layers initiate focusing of light for the eye. For best quality of vision, these layers must be smooth and regular. Unfortunately, there can be several conditions that impact the smoothness of these layers—causing irregularity. These conditions include:
-
Anterior basement membrane dystrophy (ABMD)
-
Salzmann’s nodular degeneration
-
Irregularity caused by recurrent corneal erosion (RCE)
-
Other forms of superficial corneal scarring
If you suffer from corneal diseases on the corneal surface, contact a Wolfe Eye Clinic cornea specialist near you.
Corneal Conditions That Impact the Corneal Shape
Abnormalities to the cornea’s shape, whether too flat, too step or asymmetrical can cause issues in how the cornea refracts light onto the retina, limiting your ability to focus on objects and see clearly. These conditions are known as refractive disorders and include:
Fortunately, these corneal conditions can be corrected with contact lenses, eyeglasses or LASIK laser eye surgery.
Corneal Durability
Conditions that affect the cornea’s durability can impact the cornea’s ability to maintain its shape and function. For example, keratoconus is the gradual thinning and weakening of the cornea, causing the cornea to become cone-shaped and resulting in increasingly distorted vision and blurriness over time. When the cornea’s durability is progressively impacted, procedures from a corneal specialist such as cross-linking, or a corneal transplant may be necessary to help restore its function.
Corneal Health
 Being the outer layer of the eye, the cornea is vulnerable to trauma, bacteria, and irritants such as allergens or chemicals. Since the cornea is dense with nerve fibers, it is exquisitely sensitive. This means abnormalities of the cornea can greatly affect its function and eye comfort.
Being the outer layer of the eye, the cornea is vulnerable to trauma, bacteria, and irritants such as allergens or chemicals. Since the cornea is dense with nerve fibers, it is exquisitely sensitive. This means abnormalities of the cornea can greatly affect its function and eye comfort.
Injury: Corneal abrasions can occur from objects such as glass or wood getting into the eye. Direct trauma to the cornea from a foreign object such as metal or a chemical can cause a cloudy cornea (corneal edema) or permanent corneal scarring.
Infection: Bacterial or viral infections such as conjunctivitis (pink eye) can cause discomfort and eye redness or may cause an inflamed cornea (keratitis) or even permanent scarring. Corneal infections require medical evaluation and treatment.
Irritants: Allergens and certain chemicals that make contact with the cornea can cause itchiness or pain. Typically, symptoms related to irritants appear upon contact and may require urgent medical treatment.
Patients may not know that their visual or eye comfort issues are related to the cornea. Due to the highly sensitive nature of the cornea, it is important to reach out to your eye doctor for help immediately if you are experiencing any of the following symptoms. Your doctor can help to ensure early intervention and help prevent potential damage, including referral to a cornea specialist at Wolfe Eye Clinic.
Symptoms of a cornea condition may include:
- A foreign body sensation in the eye
- Itchiness
- Redness
- Intense pain
- Burning
- Sudden vision changes
- Light sensitivity
- Blurriness or cloudiness
The cornea specialists in Iowa at Wolfe Eye Clinic can perform advanced testing to confirm any cornea irregularities. Using these test results, our cornea surgeons will then discuss possible treatments or surgical interventions that can improve your vision by increasing clarity and regularity.
What does a cornea doctor do?
No matter what’s impacting your vision, Wolfe Eye Clinic is here to help and direct you to the eye specialist you need. For corneal issues, patients are scheduled with a cornea doctor who is an  experienced ophthalmologist, many times called a cornea specialist because of the additional training they have completed in corneal disease and surgery. At the appointment, you receive a comprehensive eye exam and thorough corneal evaluation. Your Wolfe Eye Clinic cornea specialist may obtain advanced testing depending on your specific corneal issue. Together, you and your cornea doctor will discuss your concerns and develop a treatment plan to treat your vision issues and discomfort. A referral is not required for an appointment, although your optometrist or regular eye doctor may schedule you an appointment with a Wolfe Eye Clinic cornea doctor near you.
experienced ophthalmologist, many times called a cornea specialist because of the additional training they have completed in corneal disease and surgery. At the appointment, you receive a comprehensive eye exam and thorough corneal evaluation. Your Wolfe Eye Clinic cornea specialist may obtain advanced testing depending on your specific corneal issue. Together, you and your cornea doctor will discuss your concerns and develop a treatment plan to treat your vision issues and discomfort. A referral is not required for an appointment, although your optometrist or regular eye doctor may schedule you an appointment with a Wolfe Eye Clinic cornea doctor near you.
Wolfe Eye Clinic’s Cornea Specialists Lead the State of Iowa in Cornea Evaluation & Treatment
Wolfe Eye Clinic has fellowship-trained cornea specialists in Iowa serving locations across the state. We have been leaders in evaluating and treating corneal conditions and diseases including conjunctivitis, dry eye syndrome, corneal abrasions, and keratoconus, just to name a few. In 1960, Wolfe Eye Clinic was the first clinic in Iowa to offer corneal transplants outside of a University setting and we continue to offer the latest technology in treating corneal diseases. Currently, Wolfe Eye Clinic offers the most advanced cornea surgical procedures including cross-linking to treat progressive keratoconus, DMEK surgery, and topography guided LASIK laser eye surgery.
Cornea Treatment Options
While many cornea eye diseases can be solved with medical therapy from a cornea specialist, there are other conditions that require in-office procedures or surgery. Many of these treatments focus on improvement of the superficial corneal contour.
Superficial Keratectomy (SK)
SK is a surgery used to smooth the cornea. With this procedure, the irregular and diseased epithelium (outermost layer of cornea) is removed during an in-office procedure. A contact lens is used as a bandage to increase comfort. After three to four days, there is regrowth of new epithelium. Over the ensuing four weeks, the new epithelium becomes more regular. Typically, new glasses can be obtained four to six weeks after the procedure. This procedure can be helpful in conditions such as:
-
Anterior basement membrane dystrophy (ABMD)
-
Salzmann’s nodular degeneration (SND)
-
Recurrent corneal erosion (RCE)
Phototherapeutic Keratectomy (PTK)
PTK is another procedure performed to remove corneal imperfections that are in a slightly deeper layer. By using our WaveLight® EX500 Excimer Laser, the same laser used during laser vision correction surgery, Wolfe Eye Clinic corneal specialists are able to treat deeper abrasions or scar tissue. Like the superficial keratectomy (SK) procedure, PTK improves optical quality, and uses a contact lens to bandage the eye. After four to six weeks, a new glasses prescription can be obtained. This procedure can also help patients with deeper variants of anterior basement membrane dystrophy (ABMD), Salzmann’s nodular degeneration (SND), and recurrent corneal erosion (RCE).
Amniotic Membrane Transplantation (AMT)
AMT can be used to treat a variety of ocular surface conditions, such as:
- Severe dry eye
- Keratitis
- Recurrent corneal erosion
- Persistent epithelial defects
- Conjuctivochalasis
Amniotic membrane has been shown to reduce inflammation and promote healing of the ocular surface. Your cornea specialist at Wolfe Eye Clinic may use this in surgical situations and in the form of a contact lens (prokera) that could even be placed during a clinic appointment at Wolfe Eye Clinic.
Pinguecula & Pterygium Surgery
Chronically red and irritated eyes can result from a variety of causes including dry eye syndrome, blepharitis / meibomian gland dysfunction, allergic eye disease, infectious conjunctivitis (pink eye), or conjunctival degenerations. The same finding that is present in all of these red-eye causing conditions is inflammation of the blood vessels in the conjunctiva. The conjunctiva is a slippery membrane covering the white portion of the eye. It is extremely important as it secretes critical components of our tears and it contains blood vessels that supply immune elements that fight off infections. These same blood vessels can become inflamed in response to ocular irritants leading to a red eye.
The conjunctival degenerations most frequently found are pinguecula and pterygium which appear as growths on the white portion of the eye and may extend onto the cornea. These changes often lead to annoying symptoms for patients including foreign body sensation, irritation, redness or decreased vision.
Pinguecula: A conjunctival growth is labeled a pinguecula if it has a yellow-white conjunctival growth near the cornea, but not involving the cornea.
Pterygium: A conjunctival growth is labeled a pterygium if it has a blood vessel component and extends onto the cornea.
Despite their relatively common occurrence, the exact causes of pinguecula and pterygium are poorly understood. Some causes are thought to be dry eyes, elevated exposure to UV light (due to occupational or recreational habits), wind exposure, and family history.
Determining a Corneal Disease Treatment Plan with a Cornea Specialist
 For patients with few or no symptoms, a cornea specialist at Wolfe Eye Clinic may often recommend periodic examinations to make sure there is not a change in size. Medical therapy is usually recommended for patients experiencing mild symptoms. Artificial tear use is sufficient for most patients to control irritation or redness. Occasionally, your doctor may recommend use of medicated eye drops (steroids) to control inflammation. Eye drops such as Visine or Lumify can often control redness, but their use should never extend beyond three to four days due to increasing dependence and risk for rebound redness.
For patients with few or no symptoms, a cornea specialist at Wolfe Eye Clinic may often recommend periodic examinations to make sure there is not a change in size. Medical therapy is usually recommended for patients experiencing mild symptoms. Artificial tear use is sufficient for most patients to control irritation or redness. Occasionally, your doctor may recommend use of medicated eye drops (steroids) to control inflammation. Eye drops such as Visine or Lumify can often control redness, but their use should never extend beyond three to four days due to increasing dependence and risk for rebound redness.
For patients whose symptoms cannot be controlled with medical therapy or if the patient’s vision is at risk, the surgical options for these growths have never been better. For best results, either a conjunctival autograft or amniotic membrane can be used to replace the pterygium tissue that is removed.
Meet with One of Iowa’s Leading Cornea Specialists at Wolfe Eye Clinic
At Wolfe Eye Clinic, you have a team of experts providing you with the best care in the state every step of the way with locations in Ankeny, Des Moines, Fort Dodge, Hiawatha (Cedar Rapids), Iowa City, Marshalltown, Ottumwa and Pleasant Hill. If you have questions or would like to schedule an appointment with one of our corneal disease specialists, give us a call at (833) 474-5850.